The European Commission released its pharma legislation proposal in 2023 to make access to medicines more secure and affordable, encourage innovation, and reduce the gaps.
One of the key changes it proposed was to shave two years off the amount of time new branded medicines have to themselves on the market before rivals launch, down from the current eight years to six.
The newly voted in the EP text bumps that up to seven and a half years of regulatory protection, with a cap of one extra year for those that qualify.
The Parliament’s directive proposal also includes new incentives not listed in the Commission’s original text: six more months of data protection for medicines in which “significant development, including clinical and preclinical” was carried out in the EU; or for where development was done in collaboration with university hospitals, centres of excellence, or bioclusters.
The promotion of sex and gender equity has been a long standing theme in the philosophy and operations of the EU (1) and in line with Articles 160 and 168 of the Treaty on the Functioning of the European Union and the UN Sustainable Development Goals (SDGs).
It has been over 60 years since the Treaty of Rome, where gender equality was enshrined into EU law and yet no country has succeeded in reaching gender equality: this is also reflected in healthcare. The European Institute of Women’s Health (EIWH) calls on the EU to commit to the reduction of health inequalities and provide equitable health for all women, through the provision of an EU Strategy for Women’s Health.
Sex and gender impact the health and wellbeing of individuals. They can affect the risk of health problems; the efficacy and risk of adverse reactions to drugs and treatments; the metabolization of medications due to differences in physiological processes; health seeking behaviours; and interactions with health services and healthcare professionals, among other important health related factors. Women’s pain levels are more likely to be under estimated and they experience longer diagnostic delays. Women are notoriously under represented in clinical trials and as a result, they have a higher risk of experiencing an adverse reaction to a drug compared to men. All research, monitoring and evaluation data must be disaggregated by sex and gender to take into account these differences.
Many conditions specific to women lack sufficient research, attention and prioritisation, and have not received adequate funding and resources. Examples of these include polycystic ovary syndrome, which does not have a standardised treatment, and women with endometriosis experience a diagnostic delay of 7.4 years on average, despite this condition affecting 1 in 10 women. Many issues affecting girls and women across the EU continue to carry stigma and taboo in 2023 such as menopause and dysmenorrhea (painful menstruation).
The social determinants of health as well as the commercial determinants of health affect access to healthcare. Unequal opportunities, lack of decision making power, unfair work divisions and violence against women all impact health.
Women’s health is an unfinished agenda with large gaps and unmet needs persisting. Sex and gender are not systematically integrated into policy, programs, education, training, research, data collection and analysis. Existing policies, for example in the inclusion of participants in clinical trials who are representative of the population likely to use the drug or treatment, are not fully enforced. Women are the main users of health care and the main providers of that care. A comprehensive and supportive approach, must be taken by policy makers at EU and national level to empower and support women to have an active and healthy life in order to reduce inequalities.
Read the full paper here https://eurohealth.ie/2024-womens-health-manifesto/
On 20 February 2024, the Management Board of ECDC nominated Dr Pamela Rendi-Wagner to be the next Director of ECDC for a five-year period (2024-2029).

“I am delighted to announce that Dr Pamela Rendi-Wagner has been nominated to be the next ECDC Director by ECDC’s Management Board. The Board is convinced that her experience, vision and plans will serve the Centre well for the next five years. We look forward to her upcoming hearing in the European Parliament in March,” said Dr Anni Virolainen-Julkunen, Chair of the ECDC Management Board. “On behalf of the Management Board, I would also like to express our gratitude and appreciation to Dr Andrea Ammon for the excellent work she has done as ECDC Director. We wish Andrea the best as she retires in June 2024”.
Dr Pamela Rendi-Wagner spoke to ECDC staff after the vote and said “I am deeply honoured and grateful to the Management Board for entrusting me with the role of Director of ECDC. I look forward to taking up the position following the hearing at European Parliament’s Committee on Environment, Public Health and Food Safety”.
Each Management Board member had one vote, and the candidate required support from two-thirds of all voting members. The Board members cast their vote by secret ballot. The Management Board of ECDC is composed of one member designated by each Member State, two members designated by the European Parliament, and three members representing the European Commission, all with a right to vote.
Before her appointment, Dr Pamela Rendi-Wagner will be invited to make a statement before the European Parliament and to answer the questions of its Members.
Read the biography of Pamela Rendi-Wagner
Source: https://www.ecdc.europa.eu/en/news-events/new-director-ecdc-2024
EU4Health, with a budget of €5.3 billion, is the fourth and largest of the EU health programmes since their launch in 2003.
HaDEA implements the EU4Health programme by managing calls for proposals and tenders from 2021 to 2027. The programme and its calls represent an ambitious response to the COVID-19 pandemic, but go beyond crisis response to address the resilience of European healthcare systems and contribute to a healthier Europe.
Source: https://hadea.ec.europa.eu/programmes/eu4health_en
This document is the first release of the EU Data Quality Framework (DQF) for medicines regulation
and defines high-level principles and procedures that apply across EMA’s regulatory mandate. This
framework provides general considerations on data quality that are relevant for regulatory decision
making, definitions for data quality dimensions and sub-dimensions, as well as their characterisation
and related metrics. It provides an analysis of what data quality actions and metrics should be
considered in different use cases and introduces a maturity model to guide the evolution of automation
to support data-driven regulatory decision making.
This document is intended to be a general resource from which more focused recommendations can be
derived for specific regulatory domains with specified metrics and checks. See figure 1 for a
summarised representation of the key points of the DQF.
Please access the Full Document here https://www.ema.europa.eu/en/documents/regulatory-procedural-guideline/data-quality-framework-eu-medicines-regulation_en.pdf
The European Commission (EC), the Heads of Medicines Agencies (HMA) and EMA have published the first version of the Union list of critical medicines. It contains more than 200 active substances of medicines for human use considered critical for healthcare systems across the EU/EEA, for which continuity of supply is a priority and shortages should be avoided. The European medicines regulatory network will prioritise critical medicines for EU-wide actions to strengthen their supply chain.
The list is an important tool to support the EU’s efforts in ensuring supply security and preventing shortages of critical medicines. Inclusion in the list does not mean that the medicine is likely to experience a shortage in the near future. It means that the prevention of shortages is particularly important as a shortage could cause significant harm to patients and pose important challenges to health systems. A medicine is considered critical if it is used in serious diseases and cannot be easily replaced by other medicines, for example in case of a shortage. It is included in the Union list of critical medicines if it meets certain criteria, including being critical in more than one third of EU/EEA countries.
The list contains active substances covering a wide range of therapeutic areas, and includes vaccines and medicines for rare diseases. It reflects the outcome of the review of 600 active substances taken from six national lists of critical medicines . The Union list will be expanded in 2024 and will then be updated every year.
The review was carried out with all EU Member States, and criticality was assigned based on an agreed methodology developed in consultation with key stakeholder groups, including patients’ and healthcare professionals’ organisations and industry associations.
Medicines on the list can continue to be prescribed and used as usual by patients and healthcare professionals. Additional reporting requirements for marketing authorisation holders and national competent authorities will be established and become effective once the proposed pharmaceutical legislation becomes applicable.
The publication of the Union list will not impact existing or to-be-established national lists of critical medicines. However, it will support the network’s efforts in drawing up national lists where these do not yet exist. In addition, it will support and expedite the EC’s analysis of the supply chain of critical medicines to determine potential vulnerabilities, as announced in the EC’s communication of 24 October. The EC and EMA’s Medicines Shortages Steering Group (MSSG) may propose measures to address vulnerabilities in the supply of those medicines, to ultimately prevent and mitigate shortages.
More information on the list, including its composition, how it was established and how it will be used, is available in a question-and-answer document.
The Union list of critical medicines complements other measures adopted by the EMA / HMA taskforce on availability of authorised medicines and by the MSSG, such as Good practices for industry and for patients and healthcare professional organisations for the prevention of medicine shortages, the recently created MSSG solidarity mechanism, the MSSG toolkit, and the MSSG’s recommendations for actions to avoid shortages of key antibiotics used to treat respiratory infections.
MEPs adopted their recommendations on prioritising mental health, as an integral part of a person’s health, in EU and national policies.
The report, prepared by the Subcommittee on Public Health, was adopted with 59 votes in favour, six against and four abstentions. MEPs call on the Commission to draw up a long-term, comprehensive and integrated EU Mental Health Strategy, building on the recent communication, and on national governments to develop corresponding national strategies with clear timelines, adequate budgets, concrete targets and indicators to monitor progress.
Promoting mental health for all, with a focus on vulnerable groups in society
MEPs highlight that mental health and well-being are shaped by a combination of socio-economic, environmental, biological and genetic factors and that any person at any point in their life can become more susceptible to poorer mental health. A “mental-health-in-all-policies approach” is needed to prevent, address and mitigate the impact of mental health conditions, they add. The report calls on member states to prioritise and improve access to mental health services for vulnerable groups, such as children, adolescents, young adults, LGBTQIA+ persons, patients with chronic conditions and disabilities, elderly people, migrants and ethnic minorities.
Tackling discrimination, stigma and social exclusion
With mental health still stigmatised and taboo, MEPs underline that there is an urgent need to develop and implement information campaigns, raise awareness and promote open discussions of mental health conditions. The call on the Commission and EU governments to promote initiatives to combat stigma, exclusion and discrimination of people with mental health conditions, with the involvement of communities, public figures, politicians, public institutions, governments and people with lived experience.
Improving accessibility of mental health services
MEPs insist that all EU citizens must have access to the full range of quality mental health services, without financial and administrative hardship. They highlight the need to ensure further investment in public health and to address mental health workforce shortages and appropriate training.
Other key recommendations include:
- ensuring a safer and healthier digital space, to prevent online hate and cyberbullying;
- tackling gender inequalities and violence against women;
- legislative measures on the management of psychosocial risks and well-being at work;
- collecting and monitoring mental health data, as well as suicide-related data, and mapping the availability of mental health services across the EU;
- ensuring sufficient funding in future financial programs such as EU4Health and Horizon Europe, as well as a Mission on Mental Health;
- designating next year as the European Year of Mental Health, following proposal 9.1 of the Conference on the Future of Europe.
Quote
Rapporteur Sara Cerdas (S&D, PT) said: “Health policy often neglects to address mental health, which is worrisome considering the steady increase in mental health conditions. Mental health is influenced by a number of determinants, including socioeconomic factors, and is interlinked with physical health. With this first Parliament report on the matter, we urge for further EU action to address these factors, investing in prevention, support and adequate treatment for people suffering from mental health conditions and reinforcing the resilience of mental health for all.”
Background
On 7 June 2023, the Commission adopted the Communication on a comprehensive approach to mental health. It introduces 20 flagship initiatives and a holistic approach to mental health, based on adequate and effective prevention, access to high quality and affordable mental healthcare and treatment, and reintegration into society after recovery.
Abstract
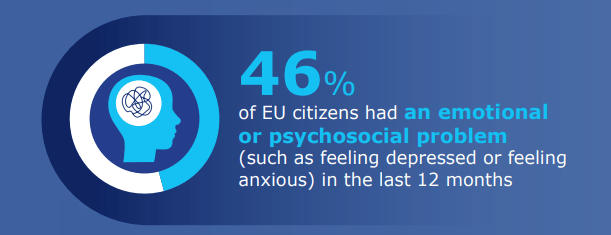
89% of respondents consider that mental health promotion is as important as physical health promotion. At the same time, less than half of respondents agree that people with mental health issues receive the same level of care as those with a physical condition. 46% of respondents have experienced an emotional or psychosocial problem, such as feeling depressed or anxious, in the past twelve months. 54% of respondents with a mental health issue have not received help from a professional. Most respondents replied that recent world events have influenced their mental health ‘somewhat’ (44%) or ‘to a great extent’ (18%).
Key findings
Mental health and recent world events
62% of EU citizens think that recent world events (the COVID-19 pandemic, the Russian aggression against Ukraine, the climate crisis, unemployment, and the food and energy costs “somewhat” or “greatly” affected their mental health.
Factors contributing to good mental health

The most important factors to achieve good mental health are living conditions (60%), followed by financial security (53%), physical activity and social contact (both 41%).
Source: https://europa.eu/eurobarometer/surveys/detail/3032
Over the past three years, EMA and the EUnetHTA 21 (European Network for Health Technology Assessment) consortium have delivered a number of milestones to prepare the EU for the entry into application of the Regulation on Health Technology Assessment. EUnetHTA 21 ceases to operate on 16 September 2023, but preparations will continue for the implementation of the Regulation, under the direction of the HTA Coordination Group.
“EMA’s collaboration with EUnetHTA began in 2010 as a project to test out whether early engagement between regulators and HTA bodies could bring tangible benefits for patient access to medicines,” said Michael Berntgen, Head of Scientific Evidence Generation Department at EMA. “Together, we were able to help medicine developers enhance clinical research and become more efficient in generating the evidence relevant for both regulatory authorities and HTA bodies.”
“Although the EMA-EUnetHTA cooperation is drawing to a close, the road does not end here,” said Niklas Hedberg, Chair of the EUnetHTA 21 Consortium Executive Board. “We are very proud to see that our cooperation has now been enshrined into European law. The experience gained provided essential technical input to shape the new legislation. In fact, we continue our joint work and will do this on a new footing, with more participants, additional responsibilities and high expectations from stakeholders.”
Reviewing achievements over the years at their concluding meeting on 14 September 2023 in Amsterdam, EMA and EUnetHTA 21 highlighted a number of initiatives:
- Completion of seven parallel joint scientific consultations (JSC) for medicines under the EUnetHTA 21 consortium contract. This joint work is intended to improve the generation of robust evidence that meets the needs of regulators and HTA bodies;
- Discussion on evidence needs for advanced therapy medicinal products in oncology, addressing mutual challenges such as indirect comparison and addressing evidence gaps through post-licensing evidence generation.
- Organisation of trainings for patients and healthcare professionals to facilitate their participation as experts in regulatory and HTA processes, alongside collaborative work on methodologies for engagement of patients and healthcare professionals in assessments;
- Recommendations to optimise the assessment reports of EMA’s Committee for Human Medicines (CHMP) for each medicine in order to systematically document key elements of the assessment such as the eligible patient population, choice of comparator and endpoints, as well as relevance of subgroup data.
More information on the achievements is available in a Report on the implementation of the EMA-EUnetHTA 21 work plan 2021 – 2023 .
The new HTA regulation
The Regulation on Health Technology Assessment (EU) 2021/228 which entered into force in January 2022 and applies as of January 2025, will govern the European cooperation between medicine regulators and HTA bodies. Under the new framework, EMA and HTA bodies will collaborate in the context of joint clinical assessments, joint scientific consultations, and the identification of emerging health technologies.
While aiming to improve the availability of innovative medicines and certain medical devices for patients in the EU, it will also ensure efficient use of resources and enhance the quality of health technology assessment in the EU by ensuring the sustainability of European cooperation. The establishment of the Member State Coordination Group on Health Technology Assessment, as provided by the regulation, and of a stakeholder network, will give a transparent and inclusive framework to facilitate continued collaboration between partners and reduce duplication of efforts for national HTA authorities and industry.
Transition period to January 2025
EMA and HTA organisations have established a new framework for Parallel EMA/HTA Scientific Advice for the period September 2023 until January 2025, when the HTA Regulation applies. During this transition period, developers can request the involvement of HTA bodies when applying for EMA scientific advice. The outcome of the procedure will be a scientific advice letter from EMA and individual written recommendations from participating HTA bodies. The selection criteria are available in the Guidance on Parallel EMA/HTA body (HTAb) Scientific Advice for the Interim Period
Preparations are also continuing at EMA to pave the way for the implementation of the Regulation. The Agency has identified a number of priorities and opportunities for the next 15 months. These include defining a single evidence plan to facilitate development programmes, harmonising views on the strength of the evidence, and involving patients, clinical experts and other relevant experts in decision-making.
Notes
- The EUnetHTA 21 consortium had been awarded the service contract for the provision of joint health technology assessment (HTA) work supporting the continuation of EU cooperation on HTA by the European Health and Digital Executive Agency (HaDEA).
The Commission’s proposal introduces a standardised European Disability Card and enhances the current European Parking Card for persons with disabilities.
Both cards will facilitate persons with disabilities to access right to free movement, by making sure they can, on an equal basis, access special conditions, preferential treatment, and parking rights when visiting another Member State.
A European Disability Card
When people’s disability status is not recognised abroad, they cannot access the special conditions and preferential treatment, such as free and/or priority access, reduced fees or personal assistance, while visiting other Member States.
To address this issue, the Commission proposes the creation of a standardised European Disability Card.
The European Disability Card will serve as recognised proof of disability throughout the EU, granting equal access to special conditions and preferential treatment in public and private services, including for instance:
- transport
- cultural events
- museums
- leisure and sport centres or amusement parks
It will be issued by the national competent authorities and complement existing national cards or certificates.

Improving the European Parking Card
For many persons with disabilities, private car transport remains the best or only possibility for travel and getting around independently, ensuring their autonomy.
The proposed improvements to the current European Parking Card will allow persons with disabilities to access the same parking rights available in another Member State.
It will have a binding common format that will replace national parking cards for persons with disabilities and be recognised throughout the EU.

Ensuring accessibility of the cards
To promote ease of use and reduce administrative burden, the proposed Directive will require Member States to:
- Provide the cards in both physical and digital versions.
- Make conditions and rules for issuing or withdrawing the cards publicly available in accessible formats.
- Ensure service providers offer information on special conditions and preferential treatment for persons with disabilities in accessible formats.
To guarantee compliance, Member States must ensure persons with disabilities, their representative organisations and relevant public bodies can take action under national law if needed.
After adoption of the Directive into national law, Member States are asked to impose fines and corrective measures in case of violations.
Next steps
The Commission’s proposal will now be discussed by the European Parliament and the Council. The proposal foresees that once adopted, Member States will have 18 months to incorporate the provisions of the Directive into national law.
Background
The proposed Directive establishing the European Disability Card and the European Parking Card for persons with disabilities was announced in the EU Strategy for the rights of persons with disabilities 2021-2030.
The proposal contributes the implementation by the EU of the United Nations Convention on the rights of persons with disabilities, to which the EU and all its Member States are party (UNCRPD).
The UNCRPD contains obligations for States Parties to recognise the rights of persons with disabilities to liberty of movement on an equal basis with others.
States Parties are also requested to take effective measures to ensure personal mobility with the greatest possible independence for persons with disabilities, including by facilitating the personal mobility of persons with disabilities in the manner and at the time of their choice, and at affordable cost.
The proposal also aligns with the principles of equal opportunities and of inclusion of people with disabilities from the European Pillar of Social Rights.
This initiative builds on the outcomes of the EU Disability Card pilot project conducted in Belgium, Cyprus, Estonia, Finland, Italy, Malta, Romania, and Slovenia between 2016 and 2018.
In addition, it integrates insights from a recent public consultation, which collected over 3,300 replies, of which 78% from persons with disabilities.
Source: https://ec.europa.eu/social/main.jsp?langId=en&catId=89&newsId=10652
